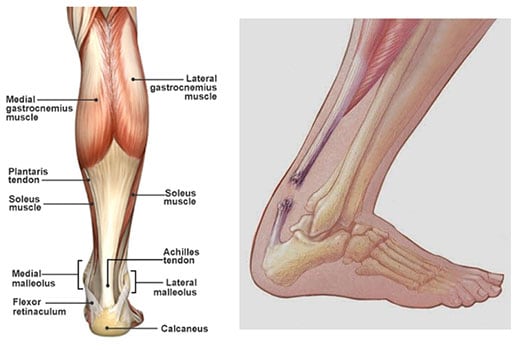
The Achilles tendon is the largest and strongest tendon in the body. As the tendon moves toward the heel, the fibers rotate, giving it greater mechanical resistance, but creating an area with poor blood supply which may makes the Achilles prone to tearing in this area.
Achilles tendon ruptures are quite common in the general population. A rupture is a break in the middle of the tendon. Most ruptures happen with athletic activities that require sudden bursts of muscle power in the legs. Patients report the rupturing sensation as being like a kick to the heel or being hit with a ball or a bat in the heel.
After a period of time the pain can sometimes go away as the tendon is not injured or strained again. This decrease in pain makes some patients feel that they did not injure themselves. Often, however, people feel weakness when pushing off with their foot to walk and difficulty going on tip-toe on that leg. Prompt evaluation and diagnosis is critical.
Sometimes MRI or ultrasound will aid in confirming the tear, but in most instances physical examination of the patient will most often provide the diagnosis; this includes the Thompson’s test.

Appearance of left Achilles rupture. Notice of loss of contour of Achilles
Watch Negative Thompson Test-Normal Achilles
Watch Positive Thompson Test-Ruptured Achilles
Once the diagnosis is made, patients have 2 treatment choices: non-surgical treatment or surgery. Non-surgical treatment can work well and is associated with fewer wound healing problems, but it does have the risk of higher rates of rupturing the tendon again and an increased recovery time. 1-2
Surgery can decrease the risk of rupturing the tendon again and is more likely to allow the tendon to again be the correct length. Having the tendon be the correct length is important so that you have the strength to walk normally once you are healed. However, surgery has two potential complications as well: slow wound healing and scar adhesions (when the skin sticks to the tendon).
Minimally-invasive Achilles tendon surgery can decrease the risks for both complications compared with traditional surgery. The surgery is performed through an inch-long incision (cut) where the tendon ends are located. A specially-designed stitch device is then passed up and around the tendon, which guides sutures (stitches) into the tendon and pulls them into the small incision. The sutures are then tied so the tendon ends meet, and when compared to the other leg, the foot and ankle should be in the same position. This means that the correct length of the tendon has been achieved.

Left: Patient 10 days after surgery. Right: Different patient 6 weeks after surgery
The minimally invasive approach:
- Avoids aggressive exposure of the tendon
- Allows a very strong repair
- Limits wound healing issues and scar tissue
- Permits a more rapid return to full activity.3
Minimally-invasive surgery is not right for every patient, depending on the condition of the tendon and where the rupture is located. The surgery and rehabilitation can be adjusted depending on these factors. The minimally invasive technique has been used quite successfully in patients, and it is a very good consideration for repair of the Achilles tendon.
*Please note that Dr. Switaj has no financial relationship or conflict of interest in relation to this product
- Nilsson-Helander K, Silbernagel KG, Thomee R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatment using validated outcome measures. Am J Sports Med. 2010;38(11):2186-2193.
- Chiodo CP, Glazebrook M, Bluman EM, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on treatment of Achilles tendon rupture. J Bone Joint Surg Am. 2010;92(14):2466-2468.
- Hsu, A et al. Clinical Outcomes and Complications of Percutaneous Achilles Repair System Versus Open Technique for Acute Achilles Tendon Ruptures. Foot Ankle Int. 2015;36(11):1279-86

