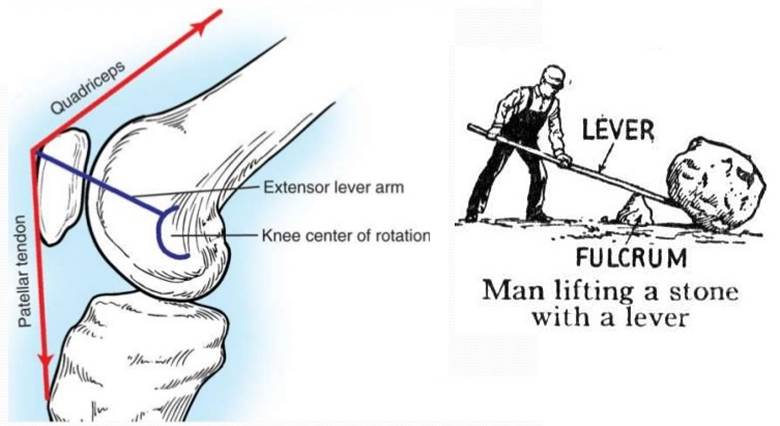
The kneecap or patella is kind of a ‘floating’ bone at the front of our knees. It’s an important structure but is vulnerable to coming out of place or dislocating. The patella is a bone embedded within the quadriceps tendon. The quadriceps tendon connects our thigh muscle to the lower leg and the patella makes the muscle more powerful by acting as a fulcrum and giving the muscle more leverage.
The patella is surrounded and stabilized by many soft tissue structures. One of the most important structures for patellar stability is called the medial patellofemoral ligament (MPFL). This is a ligament that connects the patella to the femur. I call it a “checkrein” ligament because it only tightens when the patella tries to come out of place. This structure is often injured when the kneecap dislocates. Repairing this ligament or creating a new ligament in its place has become a critical component of fixing an unstable kneecap.
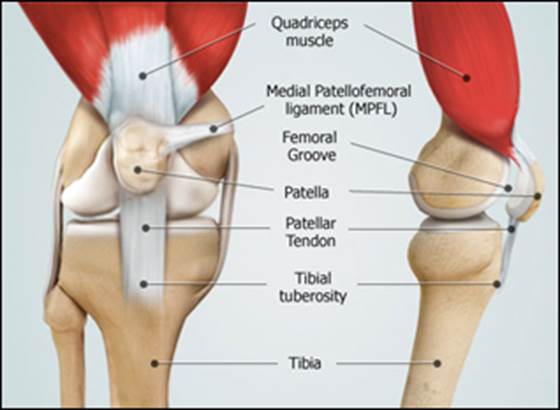
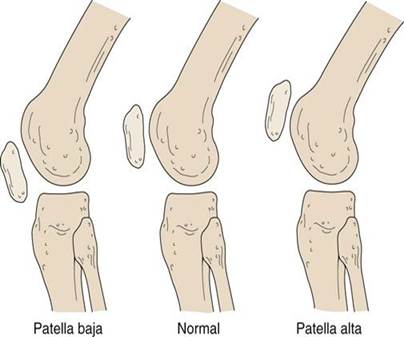
The patella is also stabilized by the bony anatomy. The bottom of our thigh bone (femur) has a special groove made specifically for the patella to glide through as our knee bends and straightens. How deep or shallow this groove is changes from person to person. A shallow groove can be a risk factor for your kneecap being unstable. Think of keeping a ball in a saucer compared to keeping it in a bowl. Which is easier? Another variable is the height of your kneecap. A kneecap that is too high (patella alta) is another risk factor for instability. This is because it doesn’t engage the groove as quickly, thereby losing the stability advantage that the bony groove provides. Other bony issues like having “knock-knees” or rotational issues with your leg bones can also predispose you to patellar instability.
The patella usually dislocates when the foot is planted and the body rotates. It almost always dislocates laterally (to the outside). It often will go back in place on its own or as soon as you straighten your knee. There can be tearing of soft tissue structures (like the MPFL), bone bruises, cartilage damage, or even fractures. Evaluation by an orthopaedic sports medicine surgeon within a week of the injury is important. The surgical treatment plan for patellar instability must take into account all the variables I’ve mentioned to have a successful outcome.

